This week’s blog post is one of utmost importance in the veterinary community – suicide in veterinarians. Not as oft-discussed as it should be, it’s becoming clearer with time that members of the veterinary medical field are prone to experiencing burnout, depression, and extreme levels of stress.
In a recent article from early September, NPR explored this topic, heading to San Francisco to speak with Dr. Carrie Jurney (DVM, DACVIM) to discuss a nonprofit she works on the board for, Not One More Vet. The statistics she discusses concerning stress and death in the field of veterinary medicine are alarming:
“The Centers for Disease Control and Prevention found male vets are 2.1 times as likely and female vets 3.5 times as likely to die by suicide compared with the general population. The much higher rate for women is especially concerning as more than 60% of vets are women.”
From a study in the AVMA journal, 400 veterinarians out of the 11,600 that have died from 1979 to 2015 died by their own hand.
Jurney even clarifies this from her own experience – out of 85 graduates in her class (2005), 3 have committed suicide.
How does this happen? Why are those in veterinary medicine so likely to take their own lives? There are a few speculated factors that can lead to this. Firstly, the stress of succeeding throughout medical school, an average $140,000 in debt for the average graduate, and median $94,000 made yearly can make for a debilitating mindset of digging out before a career even has a chance to take off.
Burnout in the medical world is extremely common, but there are several specific stressors unique to the field of veterinary medicine.
Veterinarians on average make half as much as physicians but attend schools of equally marked prestige, meaning comparable tuitions, and likelihood of student loan debt with half the efficacy of paying them off.
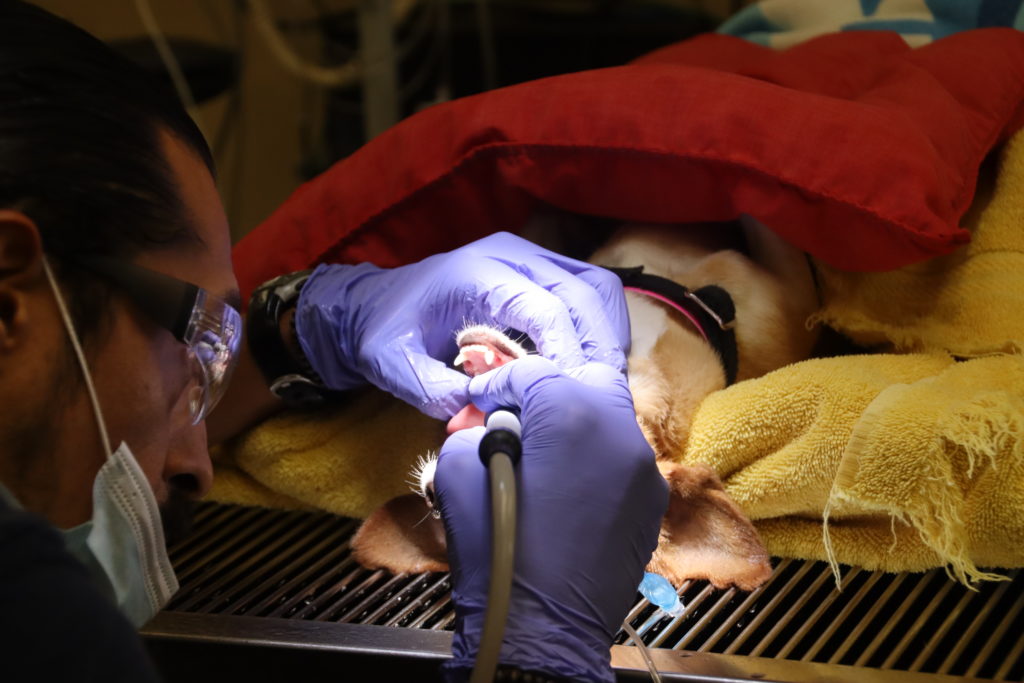
Ignoring these initial heavy obstacles into the career of the veterinarian, there is the work itself – often dealing with stressed out animals, stressed out owners, and sometimes, very dire situations.
Trying to mend the injuries and illnesses of patients who don’t know what is going on, in addition to their guardians being emotionally heightened can makes for a lot of pressure in even the most routine visits.

Coupled with long hours, underfunding, and understaffing, the day to day life of a veterinarian involves baseline stressors much higher than most medical professions.
Sometimes, there is a brief respite from these stressors when the veterinarian’s work is successful and ends in an animal leaving happy and healthy, but then again, results can be unpredictable, and the emotional investment can make for crushing lows. Immediate access to euthanasia drugs also poses a risk in conjunction with these other factors.
Jurney recalls a dog with chronic disks that she treated with emergency surgery – after many hours, the dog, unable to walk when he arrived, left walking and much improved. However, a few days later, the dog passed due to a complication from both the initial genetic problem and from the surgery to improve his disks. This was truly a painful moment for Jurney:
“I have to be honest — this is gut-wrenching. You came to us to see why the job is hard, and there is no better example than this. I am devastated. I’ve cried through many moments of my mother in law’s birthday dinner tonight because my mind is with Reuben and his poor owners. I wonder if there is anything I could have done differently. Even though I know I did everything I could for him, I still wonder if I could have done more.”
From my own conversations with veterinarians globally, an additional factor at play appears to be our professions comfort level with euthanasia. Vets are faced with making euthanasia decisions on a daily basis, unlike other medical professionals. We see animals that are suffering and in pain, have that pain and suffering relieved by end-of-life choices that their owners make and that we act upon. We are comfortable with the process of euthanasia (technically speaking) and understand what occurs from a physiological standpoint. Depending on if we are working in animal shelters or not, we may be making these choices on a daily basis on healthy and unhealthy animals alike. Death is not a foreign concept to veterinarians. It is one that they discuss and internalize on a daily basis in their work.
Isolation can also take its toll – due to the aforementioned long hours, and sometimes geographically, the veterinarian in question will be hundreds of miles from another vet, meaning they are the only professional in the area licensed to care for animals. Even still, many practice alone – making for even busier, more stressful, and lonely careers.
In an ironic twist of fate, data collection by Kim Repp and medical examiner Charles Lovato shows a peculiar cycle where in some instances, suicidal people will bring all their animals to a shelter. This happens frequently enough that those in the shelter and veterinary community often undergo training to recognize the signs of stress and depression that can lead to suicide, with no avail in the numbers they lose themselves.
This trend of the veterinary community subjecting themselves more and more to stress and isolation is directly linked to the higher rates of suicide, depression, and anxiety. Luckily, there are important ways to create a capacity of care for members of the veterinary community.

Nicole McArthur, founder of Not One More Vet, works to provide a safe place for veterinarians who understand the stress of the industry to speak with each other, share their insights, feelings and worries, and create a network of care and support.
The more networks that allow for veterinarians to share their feelings and feel heard by others who understand the struggle, the easier it will be to destigmatize these hardships of the industry and work together to find solutions and self care.
There are also methods that veterinarians can utilize in their day to day lives to create a capacity to care for themselves the same way they care for their patients. More to come on that soon!


